Thyroid nodule
| Thyroid nodule | |
|---|---|
 | |
| Human thyroid with cancer nodules | |
| Classification and external resources | |
| Specialty | endocrinology |
| ICD-10 | E04.1 |
| ICD-9-CM | 241.0 |
| DiseasesDB | 5332 |
| MedlinePlus | 007265 |
| eMedicine | med/3224 |
| MeSH | D016606 |
Thyroid nodules are lumps which commonly arise within an otherwise normal thyroid gland.[1] They indicate a thyroid neoplasm, but only a small percentage of these are thyroid cancers.
Presentation
Often these abnormal growths of thyroid tissue are located at the edge of the thyroid gland and can be felt as a lump in the throat. When they are large or when they occur in very thin individuals, they can sometimes be seen as a lump in the front of the neck.
Sometimes a thyroid nodule presents as a fluid-filled cavity called a thyroid cyst. Often, solid components are mixed with the fluid. Thyroid cysts most commonly result from degenerating thyroid adenomas, which are benign, but they occasionally contain malignant solid components.[2]
Diagnosis
After a nodule is found during a physical examination, a referral to an endocrinologist, a thyroidologist or otolaryngologist may occur. Most commonly an ultrasound is performed to confirm the presence of a nodule, and assess the status of the whole gland. Measurement of thyroid stimulating hormone and anti-thyroid antibodies will help decide if there is a functional thyroid disease such as Hashimoto's thyroiditis present, a known cause of a benign nodular goitre.[3] Fine needle biopsy for histopathology is also used.[4][5]
Thyroid nodules are extremely common in young adults and children. Almost 50% of people have had one, but they are usually only detected by a physician during the course of a health examination or fortuitously discovered during the investigation of an unrelated condition.[6]
Fine needle biopsy
One approach used to determine whether the nodule is malignant is the fine needle biopsy (FNB),[4] which some have described as the most cost-effective, sensitive and accurate test.[7][8] FNB or ultrasound-guided FNA usually yields sufficient thyroid cells to assess the risk of malignancy, although in some cases, the suspected nodule may need to be removed surgically for pathological examination. The report may be done according to the Bethesda System for Reporting Thyroid Cytopathology.
Blood tests
Blood or imaging tests may be done prior to or in lieu of a biopsy. The possibility of a nodule which secretes thyroid hormone (which is less likely to be cancer) or hypothyroidism is investigated by measuring thyroid stimulating hormone (TSH), and the thyroid hormones thyroxine (T4) and triiodothyronine (T3).
Tests for serum thyroid autoantibodies are sometimes done as these may indicate autoimmune thyroid disease (which can mimic nodular disease).
Imaging
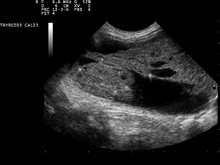
The blood assays may be accompanied by ultrasound imaging of the nodule to determine the position, size and texture, and to assess whether the nodule may be cystic (fluid filled). Also suspicious findings in a nodule are hypoechoic,[9] irregular borders, microcalcifications, or very high levels of blood flow within the nodule. Less suspicious findings in benign nodules include, hyperechoic, comet tail artifacts from colloid, no blood flow in the nodule and a halo, or smooth border.
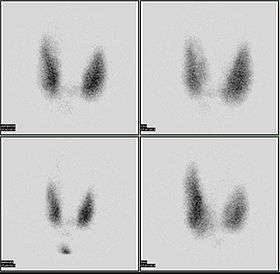
Nuclear medicine can be used to image the thyroid with radioactive technetium (Tc) or iodine (I) imaging of the thyroid.[10] An 123I scan showing a hot nodule, accompanied by a lower than normal TSH, is strong evidence that the nodule is not cancerous, as most hot nodules are benign.
Malignancy
Only a small percentage of lumps in the neck are malignant (around 4 – 6.5%[11]), and most thyroid nodules are benign colloid nodules.
There are many factors to consider when diagnosing a malignant lump. Trouble swallowing or speaking, swollen cervical lymph nodes or a firm, immobile nodule are more indicative of malignancy, whereas a family history of autoimmune disease or goiter, thyroid hormonal dysfunction or a soft, painful nodule are more indicative of benignancy.
The prevalence of cancer is higher in males, patients under 20 years old or over 70 years old, and patients with a history of head and neck irradiation or a family history of thyroid cancer.[12]
Solitary thyroid nodule
Risks for cancer
Solitary thyroid nodules are more common in females yet more worrisome in males. Other associations with neoplastic nodules are family history of thyroid cancer and prior radiation to the head and neck. Most common cause of solitary thyroid nodule is benign colloid nodules and second most common cause is follicular adenoma.[13]
Radiation exposure to the head and neck may be for historic indications such as tonsillar and adenoid hypertrophy, "enlarged thymus", acne vulgaris, or current indications such as Hodgkin's lymphoma. Children living near the Chernobyl nuclear power plant during the catastrophe of 1986 have experienced a 60-fold increase in the incidence of thyroid cancer. Thyroid cancer arising in the background of radiation is often multifocal with a high incidence of lymph node metastasis and has a poor prognosis.
Signs and symptoms
Worrisome sign and symptoms include voice hoarseness, rapid increase in size, compressive symptoms (such as dyspnoea or dysphagia) and appearance of lymphadenopathy.
Investigations
- TSH – A thyroid-stimulating hormone level should be obtained first. If it is suppressed, then the nodule is likely a hyperfunctioning (or "hot") nodule. These are rarely malignant.
- FNAC – fine needle aspiration cytology is the investigation of choice given a non-suppressed TSH. Repeat the FNAC in 6 months if the nodule enlarges.
- Imaging – Ultrasound and radioiodine scanning.
Thyroid scan
- Cold – 85% of nodules are cold. 5–8% of cold and warm nodules are malignant.[14]
- Hot – 5% of nodules are hot. Malignancy is virtually nonexistent in hot nodules.[15]
Surgery
Surgery (thyroidectomy) may be indicated in the following instances:
- Reaccumulation of the nodule despite 3–4 repeated FNACs
- Size in excess of 4 cm in some cases
- Compressive symptoms
- Signs of malignancy (vocal cord dysfunction, lymphadenopathy)
- Cytopathology that does not exclude thyroid cancer
Treatment
Levothyroxine is a stereoisomer of thyroxine which is degraded much slower and can be administered once daily in patients with hypothyroidism.
See also
| Wikimedia Commons has media related to Thyroid nodule. |
References
- ↑ "New York Thyroid Center: Thyroid Nodules".
- ↑ mayoclinic.com > Thyroid nodules Feb. 22, 2011
- ↑ Bennedbaek FN, Perrild H, Hegedüs L (1999). "Diagnosis and treatment of the solitary thyroid nodule. Results of a European survey". Clin. Endocrinol. (Oxf). 50 (3): 357–63. doi:10.1046/j.1365-2265.1999.00663.x. PMID 10435062.
- 1 2 Ravetto C, Colombo L, Dottorini ME (2000). "Usefulness of fine-needle aspiration in the diagnosis of thyroid carcinoma: a retrospective study in 37,895 patients". Cancer. 90 (6): 357–63. doi:10.1002/1097-0142(20001225)90:6<357::AID-CNCR6>3.0.CO;2-4. PMID 11156519.
- ↑ "Thyroid Nodule".
- ↑ Russ G (Sep 2014). "Thyroid incidentalomas: epidemiology, risk stratification with ultrasound and workup". European Thyroid Journal. 3: 154–63. doi:10.1159/000365289. PMID 25538897.
- ↑ Hamberger, B (1982). "Fine-needle aspiration biopsy of thyroid nodules. Impact on thyroid practice and cost of care". Am J Med. 73 (3): 381–384. doi:10.1016/0002-9343(82)90731-8. PMID 7124765.
- ↑ Mazzaferri (1993). "Management of a Solitary Thyroid Nodule". N Engl J Med. 328 (8): 553–9. doi:10.1056/NEJM199302253280807. PMID 8426623.
- ↑ Wong KT, Ahuja AT (2005). "Ultrasound of thyroid cancer". Cancer Imaging. 5: 157–66. doi:10.1102/1470-7330.2005.0110. PMC 1665239
 . PMID 16361145.
. PMID 16361145. - ↑ MedlinePlus Encyclopedia Thyroid scan
- ↑ http://www.uptodate.com/contents/diagnostic-approach-to-and-treatment-of-thyroid-nodules?source=search_result&search=thyroid+nodule&selectedTitle=1%7E100[]
- ↑ Thyroid Nodule at eMedicine
- ↑ Schwartz 7th/e page 1679,1678
- ↑ Gates, Jeremy D.; Benavides, Linda C.; Shriver, Craig D.; Peoples, George E.; Stojadinovic, Alexander (2009). "Preoperative Thyroid Ultrasound In All Patients Undergoing Parathyroidectomy?". Journal of Surgical Research. 155 (2): 254–60. doi:10.1016/j.jss.2008.09.012. PMID 19482296.
- ↑ Robbins pathology 8ed page 767