Oxendolone
 | |
| Clinical data | |
|---|---|
| Trade names | Prostetin |
| Pharmacokinetic data | |
| Biological half-life | 5–6 days (intramuscular)[1] |
| Identifiers | |
| |
| CAS Number | 33765-68-3 |
| PubChem (CID) | 36592 |
| ChemSpider | 392001 |
| Chemical and physical data | |
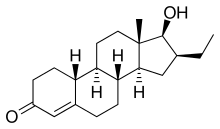
| Formula | C20H30O2 |
| Molar mass | 302.451 g/mol |
| 3D model (Jmol) | Interactive image |
| |
| |
Oxendolone (INN, USAN, JAN) (brand name Prostetin; former developmental code name TSAA-291), also known as 16β-ethyl-19-nortestosterone or 16β-ethylestr-4-en-17β-ol-3-one, is a steroidal antiandrogen and progestin of the 19-nortestosterone group that has been marketed in Japan by Takeda for the treatment of benign prostatic hyperplasia (BPH) since 1981.[2][3][4][5] It binds to the androgen receptor (AR) (Ki = 320 nM) and progesterone receptor (Ki = 20 nM) and acts as a weak but clinically relevant inhibitor of 5α-reductase (IC50 = 1.4 μM).[6][7][8][9] The binding affinity of oxendolone for the AR is far lower than that of cyproterone acetate.[1] At the AR, oxendolone is not a silent antagonist but is rather predominantly antagonistic with weak agonistic activity;[7] for this reason, it has been described as a selective androgen receptor modulator.[10] The drug has antigonadotropic properties via its progestogenic actions.[11] Although oxendolone is approved for the treatment of BPH in Japan, concerns have been raised about its use for this condition due to poor efficacy seen in clinical trials.[5]
See also
References
- 1 2 Gao, Wenqing; Bohl, Casey E.; Dalton, James T. (2005). "Chemistry and Structural Biology of Androgen Receptor". Chemical Reviews. 105 (9): 3352–3370. doi:10.1021/cr020456u. ISSN 0009-2665.
- ↑ J. Elks (14 November 2014). The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. Springer. pp. 914–. ISBN 978-1-4757-2085-3.
- ↑ William Andrew Publishing (22 October 2013). Pharmaceutical Manufacturing Encyclopedia, 3rd Edition. Elsevier. pp. 2935–. ISBN 978-0-8155-1856-3.
- ↑ Tan, MH Eileen; Li, Jun; Xu, H Eric; Melcher, Karsten; Yong, Eu-leong (2014). "Androgen receptor: structure, role in prostate cancer and drug discovery". Acta Pharmacologica Sinica. 36 (1): 3–23. doi:10.1038/aps.2014.18. ISSN 1671-4083.
- 1 2 Ishizuka, Osamu; Nishizawa, Osamu; Hirao, Yoshihiko; Ohshima, Shinichi (2002). "Evidence-based meta-analysis of pharmacotherapy for benign prostatic hypertrophy". International Journal of Urology. 9 (11): 607–612. doi:10.1046/j.1442-2042.2002.00539.x. ISSN 0919-8172.
- ↑ Annual Reports in Medicinal Chemistry. Academic Press. 8 September 1989. pp. 199–. ISBN 978-0-08-058368-6.
- 1 2 Annual report of Shionogi Research Laboratories. 1991. pp. 76–77.
- ↑ Kirby, RogerS.; Christmas, Timothy (1991). "The potential value of 5-alpha-reductase inhibition in the treatment of bladder outflow obstruction due to benign prostatic hyperplasia". World Journal of Urology. 9 (1). doi:10.1007/BF00184713. ISSN 0724-4983.
- ↑ Bashirelahi, N.; Ganesan, S.; Ekiko, D.B.; Young, J.D.; Shida, K.; Yamanaka, H.; Takahashi, E. (1986). "Effect of 16β-ethyl-17β-hydroxy-4-estren-3-one (tsaa-291) on the binding of promegestone (r5020) and methyltrienolone (r1881) to hyperplastic and neoplastic human prostate". Journal of Steroid Biochemistry. 25 (3): 367–374. doi:10.1016/0022-4731(86)90249-9. ISSN 0022-4731.
- ↑ Hikichi, Yukiko; Yamaoka, Masuo; Kusaka, Masami; Hara, Takahito (2015). "Selective androgen receptor modulator activity of a steroidal antiandrogen TSAA-291 and its cofactor recruitment profile". European Journal of Pharmacology. 765: 322–331. doi:10.1016/j.ejphar.2015.08.052. ISSN 0014-2999.
- ↑ Sudo, K.; Yamazaki, I.; Masuoka, M.; Nakayama, R. (1979). "IV. EFFECTS OF THE ANTI-ANDROGEN TSAA-291 (16 -ETHYL-17 -HYDROXY-4-OESTREN-3-ONE) ON THE SECRETION OF GONADOTROPHINS". European Journal of Endocrinology. 92 (3 Supplb): S53–S66. doi:10.1530/acta.0.092S053. ISSN 0804-4643.