Hydronephrosis
| Hydronephrosis | |
|---|---|
|
Specimen of a kidney that has undergone extensive dilation due to hydronephrosis. Note the extensive atrophy and thinning of the renal cortex. | |
| Classification and external resources | |
| Specialty | Urology, nephrology |
| ICD-10 | N13.0-N13.3 |
| ICD-9-CM | 591 |
| DiseasesDB | 6145 |
| MedlinePlus | 000506 000474 |
| MeSH | D006869 |
Hydronephrosis—literally "water inside the kidney"—refers to distension and dilation of the renal pelvis and calyces, usually caused by obstruction of the free flow of urine from the kidney. Untreated, it leads to progressive atrophy of the kidney.[1] One or both kidneys may be affected.[2] In cases of hydroureteronephrosis, there is distention of both the ureter and the renal pelvis and calices.[3]
Signs and symptoms
The signs and symptoms of hydronephrosis depend upon whether the obstruction is acute or chronic, partial or complete, unilateral or bilateral. Hydronephrosis that occurs acutely with sudden onset (as caused by a kidney stone) can cause intense pain in the flank area (between the hips and ribs). Historically, this type of pain has been described as "Dietl's crisis".[4][5] Conversely, hydronephrosis that develops gradually will generally cause either attacks of a dull discomfort or no pain. Nausea and vomiting may also occur. An obstruction that occurs at the urethra or bladder outlet can cause pain and pressure resulting from distension of the bladder. Blocking the flow of urine will commonly result in urinary tract infections which can lead to the development of additional stones, fever, and blood or pus in the urine. If complete obstruction occurs, kidney failure may follow.[6]
Blood tests may show impaired kidney function (elevated urea or creatinine) or electrolyte imbalances such as hyponatremia or hyperchloremic metabolic acidosis. Urinalysis may indicate an elevated pH due to the secondary destruction of nephrons within the affected kidney. Physical examination may detect a palpable abdominal or flank mass caused by the enlarged kidney.
Causes
Hydronephrosis is the result of any of several abnormal pathophysiological occurrences. Structural abnormalities of the junctions between the kidney, ureter, and bladder that lead to hydronephrosis can occur during fetal development. Some of these congenital defects have been identified as inherited conditions, however the benefits of linking genetic testing to early diagnosis have not been determined.[7] Other structural abnormalities could be caused by injury, surgery, or radiation therapy.
Compression of one or both ureters can also be caused by other developmental defects not completely occurring during the fetal stage such as an abnormally placed vein, artery, or tumor. Bnhbilateral compression of the ureters can occur during pregnancy due to enlargement of the uterus. Changes in hormone levels during this time may also affect the muscle contractions of the bladder, further complicating this condition.
Sources of obstruction that can arise from other various causes include kidney stones, blood clots, or retroperitoneal fibrosis.[8]
The obstruction may be either partial or complete and can occur anywhere from the urethral meatus to the calyces of the renal pelvis.Hydronephrosis can also result from the reverse flow of urine from the bladder back into the kidneys. This reflux can be caused by some of the factors listed above as well as compression of the bladder outlet into the urethra by prostatic enlargement or impaction of feces in the colon, as well as abnormal contractions of bladder muscles resulting from neurological dysfunction or other muscular disorders.[6]
Pathophysiology
Obstruction that occurs anywhere along the upper urinary tract will lead to increased pressure within the structures of the kidney due to the inability to pass urine from the kidney to the bladder. Common causes of upper tract obstruction include obstructing stones and ureteropelvic junction (UPJ) obstruction caused by intrinsic narrowing of the ureters or an overlying vessel.
Obstruction occurring in the lower urinary tract can also cause this increased pressure through the reflux of urine into the kidney. Common causes include bladder dysfunction (such as neurogenic bladder) and urethral obstruction (such as posterior urethral valves in male infants) or compression (such as from prostatic hypertrophy in older male adults).
Anything that causes obstruction leads to increased pressure being transmitted to the delicate tissues that make up the filtration system within the kidneys, which could eventually result in infection, stone formation, or loss of function. Additional complications arising from obstruction of the lower urinary tract include the stagnation of urine flow which can also lead to infection in the bladder. Obstruction may be a result of a tumour in the pelvis compressing the ureters or urethra, for example in patients with advanced cervical cancer (stage IIIA to IVB).
Diagnosis


Prenatal diagnosis is possible,[9] and in fact, most cases in pediatric patients are incidentally detected by routine screening ultrasounds obtained during pregnancy.[10] However, approximately half of all prenatally identified hydronephrosis is transient, and resolves by the time the infant is born, and in another 15%, the hydronephrosis persists but is not associated with urinary tract obstruction (so-called non-refluxing, non-obstructive hydronephrosis). For these children, regression of the hydronephrosis occurs spontaneously, usually by age 3. However, in the remaining 35% of cases of prenatal hydronephrosis, a pathological condition can be identified postnatally.[11]
Diagnostic workup depends on the age of the patient, as well as whether the hydronephrosis was detected incidentally or prenatally or is associated with other symptoms.Blood tests (such measurement of creatinine) are typically indicated, though they must be interpreted cautiously. Even in cases of severe unilateral hydronephrosis, the overall kidney function may remain normal since the unaffected kidney will compensate for the obstructed kidney.
Urinalysis is usually performed to determine the presence of blood (which is typical for kidney stones) or signs of infection (such as a positive leukocyte esterase or nitrite). Impaired concentrating ability or elevated urine pH (distal renal tubular acidosis) are also commonly found due to tubular stress and injury.
Imaging studies
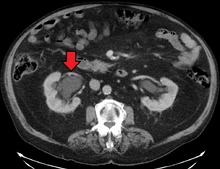
Imaging studies, such as an intravenous urogram (IVU), ultrasound, CT or MRI, are also important investigations in determining the presence and/ or cause of hydronephrosis. Whilst ultrasound allows for visualisation of the ureters and kidneys (and determine the presence of hydronephrosis and / or hydroureter), an IVU is useful for assessing the anatomical location of the obstruction. Antegrade or retrograde pyelography will show similar findings to an IVU but offer a therapeutic option as well. Real-time ultrasounds and color-flow Doppler tests in association with vascular resistance testing helps determine how a given obstruction is effecting urinary functionality in hydronephrotic patients.[12]

In determining the cause of hydronephrosis, it is important to rule out urinary obstruction. One way to do this is to test the kidney function. This can be done by, for instance, a diuretic intravenous pyelogram, in which the urinary system is observed radiographically after administration of a diuretic, such as 5% mannitol, and an intravenous iodine contrast.[13] The location of obstruction can be determined with a Whittaker (or pressure perfusion) test, wherein the collecting system of the kidney is accessed percutaneously, and the liquid is introduced at high pressure and constant rate of 10ml/min while measuring the pressure within the renal pelvis. A rise in pressure above 22 cm H2O suggests that the urinary collection system is obstructed. When arriving at this pressure measurement, bladder pressure is subtracted from the initial reading of internal pressure. (The test was first described by Whittaker in 1973 to test the hypothesis that patients' whose hydronephrosis persists after the posterior urethral valves have been ablated usually have ureters that are not obstructed, even though they may be dilated.)[12]
Kay recommends that a neonate born with untreated in utero hydronephrosis receive a renal ultrasound within two days of birth. A renal pelvis greater than 12mm in a neonate is considered abnormal and suggests significant dilation and possible abnormalities such as obstruction or morphological abnormalities in the urinary tract.[12]
The choice of imaging depends on the clinical presentation (history, symptoms and examination findings). In the case of renal colic (one sided loin pain usually accompanied by a trace of blood in the urine) the initial investigation is usually a spiral or helical CT scan. This has the advantage of showing whether there is any obstruction of flow of urine causing hydronephrosis as well as demonstrating the function of the other kidney. Many stones are not visible on plain X-ray or IVU but 99% of stones are visible on CT and therefore CT is becoming a common choice of initial investigation. CT is not used however, when there is a reason to avoid radiation exposure, e.g. in pregnancy.
For incidentally detected prenatal hydronephrosis, the first study to obtain is a postnatal renal ultrasound, since as noted, many cases of prenatal hydronephrosis resolve spontaneously. This is generally done within the first few days after birth, although there is some risk that obtaining an imaging study this early may miss some cases of mild hydronephrosis due to the relative oliguria of a newborn. Thus, some experts recommend obtaining a follow up ultrasound at 4–6 weeks to reduce the false-negative rate of the initial ultrasound.[14] A voiding cystourethrogram (VCUG) is also typically obtained to exclude the possibility of vesicoureteral reflux or anatomical abnormalities such as posterior urethral valves. Finally, if hydronephrosis is significant and obstruction is suspected, such as a ureteropelvic junction (UPJ) or ureterovesical junction (UVJ) obstruction, a nuclear imaging study such as a MAG-3 scan is warranted.
Grading
The Society of Foetal Ultrasound has developed a grading system, which was intended for use with neonatal and infant hydronephrosis, which is now used for grading hydronephrosis.
- Grade 0 – no dilation with calyceal walls apposed
- Grade 1 (mild) – dilation of the renal pelvis without dilation of the calyces nor parenchymal atrophy
- Grade 2 (mild) – dilation of the renal pelvis and calyces without parenchymal atrophy
- Grade 3 (moderate) – moderate dilation of the renal pelvis and calyces with blunting of the fornicies and flattening of papillae
- Grade 4 (severe) – gross dilation/ballooning of the renal pelvis and calyces with loss of borders between the renal pelvis and calyces and renal atrophy seen as cortical thinning
Treatment


Treatment of hydronephrosis focuses upon the removal of the obstruction and drainage of the urine that has accumulated behind the obstruction. Therefore, the specific treatment depends upon where the obstruction lies, and whether it is acute or chronic.
Acute obstruction of the upper urinary tract is usually treated by the insertion of a nephrostomy tube. Chronic upper urinary tract obstruction is treated by the insertion of a ureteric stent or a pyeloplasty.
Lower urinary tract obstruction (such as that caused by bladder outflow obstruction secondary to prostatic hypertrophy) is usually treated by insertion of a urinary catheter or a suprapubic catheter.Surgery is not required in all prenatally detected cases.[15]
Prognosis
The prognosis of hydronephrosis is extremely variable, and depends on the condition leading to hydronephrosis, whether one (unilateral) or both (bilateral) kidneys are affected, the pre-existing kidney function, the duration of hydronephrosis (acute or chronic), and whether hydronephrosis occurred in developing or mature kidneys.
For example, unilateral hydronephrosis caused by an obstructing stone will likely resolve when the stone passes, and the likelihood of recovery is excellent. Alternately, severe bilateral prenatal hydronephrosis (such as occurs with posterior urethral valves) will likely carry a poor long-term prognosis, because obstruction while the kidneys are developing causes permanent kidney damage even if the obstruction is relieved postnatally.
References
- ↑ Kumar, Vinay; Fausto, Nelson; Fausto, Nelso; Robbins, Stanley L.; Abbas, Abul K.; Cotran, Ramzi S. (2005). Robbins and Cotran Pathologic Basis of Disease (7th ed.). Philadelphia PA: Elsevier Saunders. pp. 1012–4. ISBN 0-7216-0187-1.
- ↑ Tamparo, Carol (2011). Fifth Edition: Diseases of the Human Body. Philadelphia, PA: F. A. Davis Company. p. 441. ISBN 978-0-8036-2505-1.
- ↑ NDI Foundation: hydroureteronephrosis Retrieved on Jan 4, 2009
- ↑ "Dietl's crisis". medcyclopaedia.com. 2012. Retrieved 2012-05-01.
- ↑ Mergener, K; et al. (December 1997). "Dietl's crisis: a syndrome of episodic abdominal pain of urologic origin that may present to a gastroenterologist". Am J Gastroenterol. 92 (12): 2289–91. PMID 9399772.
- 1 2 "Hydronephrosis: Merck Manuals Home Health Handbook". New Jersey: Merck and Co., Inc. 2009. Retrieved November 5, 2010.
- ↑ Toka HR, Toka O, Hariri A, Nguyen HT (July 2010). "Congenital anomalies of kidney and urinary tract". Semin. Nephrol. 30 (4): 374–86. doi:10.1016/j.semnephrol.2010.06.004. PMID 20807610.
- ↑ Koh JS, Wong MY, Li MK, Foo KT (September 1998). "Idiopathic retroperitoneal fibrosis with bilateral lower ureteric obstruction—a case report with literature review". Singapore Med J. 39 (9): 416–7. PMID 9885722.
- ↑ Estrada CR (July 2008). "Prenatal hydronephrosis: early evaluation". Current Opinion in Urology. 18 (4): 401–3. doi:10.1097/MOU.0b013e328302edfe. PMID 18520762.
- ↑ Woodward, M; Frank, D (January 2002). "Postnatal management of antenatal hydronephrosis". BJU Int. 89 (2): 149–156. doi:10.1046/j.1464-4096.2001.woodward.2578.x. PMID 11849184.
- ↑ Carmody, JB; Carmody, RB (December 2011). "Question from the clinician: management of prenatal hydronephrosis". Pediatr Rev. 32 (12): e110–2. doi:10.1542/pir.32-12-e110. PMID 22135428.
- 1 2 3 Kay, Robert, M.D. "Evaluation of Hydronephrosis in Children" in Urology Secrets, 2nd Ed. by Resnick & Novick; 1999, Hanley & Belfus
- ↑ Dr. Asmita Parikh LCEH (Bom)., "Intravenous Pyelography"; Indian Journal of Homeopathic Medicine, Vol 31, No 2; available at homeoint.org
- ↑ Aksu, N; et al. (September 2005). "Postnatal management of infants with antenatally detected hydronephrosis". Pediatr Nephrol. 20 (9): 1253–9. doi:10.1007/s00467-005-1989-3. PMID 16025288.
- ↑ Onen A (December 2007). "Treatment and outcome of prenatally detected newborn hydronephrosis". J Pediatr Urol. 3 (6): 469–76. doi:10.1016/j.jpurol.2007.05.002. PMID 18947797.
External links
- Hydronephrosis Diagnosis and Treatment at SSM Health St. Louis Fetal Care Institute
- Hydronephrosis symptoms, diagnosis, treatment and general information
