Xerostomia
| Xerostomia | |
|---|---|
| Classification and external resources | |
| ICD-10 | K11.7, R68.2 |
| ICD-9-CM | 527.7 |
| DiseasesDB | 17880 |
| Patient UK | Xerostomia |
| MeSH | D014987 |
Xerostomia (also termed dry mouth[1] as a symptom or dry mouth syndrome[2] as a syndrome) is dryness in the mouth (xero- + stom- + -ia), which may be associated with a change in the composition of saliva, or reduced salivary flow (hyposalivation), or have no identifiable cause.
This symptom is very common and is often seen as a side effect of many types of medication. It is more common in older people (mostly because this group tend to take several medications) and in persons who breathe through their mouths (mouthbreathing). Dehydration, radiotherapy involving the salivary glands, and several diseases can cause hyposalivation or a change in saliva consistency and hence a complaint of xerostomia. Sometimes there is no identifiable cause, and there may be a psychogenic reason for the complaint.[1]
Definition
Xerostomia is the subjective feeling of oral dryness, which is often (but not always) associated with hypofunction of the salivary glands.[3] The term is derived from the Greek words ξηρός (xeros) meaning "dry" and στόμα (stoma) meaning "mouth".[4][5] Hyposalivation is a clinical diagnosis that is made based on the history and examination,[1] but reduced salivary flow rates have been given objective definitions. Salivary gland hypofunction has been defined as any objectively demonstrable reduction in whole and/or individual gland flow rates.[6] An unstimulated whole saliva flow rate in a normal person is 0.3–0.4 ml per minute,[7] and below 0.1 ml per minute is significantly abnormal. A stimulated saliva flow rate less than 0.5 ml per gland in 5 minutes or less than 1 ml per gland in 10 minutes is decreased.[1] The term subjective xerostomia is sometimes used to describe the symptom in the absence of any detectable abnormality or cause.[8] Xerostomia may also result from a change in composition of saliva (from serous to mucous).[6] Salivary gland dysfunction is an umbrella term for the presence of either xerostomia or salivary gland hypofunction.[6]
Signs and symptoms
True hyposalivation may give the following signs and symptoms:
- Dental caries (xerostomia related caries) – Without the anticariogenic actions of saliva, tooth decay is a common feature and may progress much more aggressively than it would otherwise ("rampant caries"). It may affect tooth surfaces that are normally spared, e.g., cervical caries and root surface caries. This is often seen in patients who have had radiotherapy involving the major salivary glands, termed radiation-induced caries.[9]
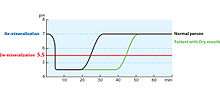
- Acid erosion. Saliva acts as a buffer and helps to prevent demineralization of teeth.[10]
- Oral candidiasis – A loss of the antimicrobial actions of saliva may also lead to opportunistic infection with Candida species.[9]
- Ascending (suppurative) sialadenitis – an infection of the major salivary glands (usually the parotid gland) that may be recurrent.[3] It is associated with hyposalivation, as bacteria are able to enter the ductal system against the diminished flow of saliva.[7] There may be swollen salivary glands even without acute infection, possibly caused by autoimmune involvement.[3]
- Dysgeusia – altered taste sensation (e.g., a metallic taste)[1] and dysosmia, altered sense of smell.[3]
- Intraoral halitosis[1] – possibly due to increased activity of halitogenic biofilm on the posterior dorsal tongue (although dysgeusia may cause a complaint of nongenuine halitosis in the absence of hyposalivation).
- Oral dysesthesia – a burning or tingling sensation in the mouth.[1][3]
- Saliva that appears thick or ropey.[9]
- Mucosa that appears dry.[9]
- A lack of saliva pooling in the floor of the mouth during examination.[1]
- Dysphagia – difficulty swallowing and chewing, especially when eating dry foods. Food may stick to the tissues during eating.[9]
- The tongue may stick to the palate,[7] causing a clicking noise during speech, or the lips may stick together.[1]
- Gloves or a dental mirror may stick to the tissues.[9]
- Fissured tongue with atrophy of the filiform papillae and a lobulated, erythematous appearance of the tongue.[1][9]
- Saliva cannot be "milked" (expressed) from the parotid duct.[1]
- Difficulty wearing dentures, e.g., when swallowing or speaking.[1] There may be generalized mucosal soreness and ulceration of the areas covered by the denture.[3]
- Mouth soreness and oral mucositis.[1][3]
- Lipstick or food may stick to the teeth.[1]
- A need to sip drinks frequently while talking or eating.[3]
- Dry, sore, and cracked lips and angles of mouth.[3]
- Thirst.[3]
However, sometimes the clinical findings do not correlate with the symptoms experienced.[9] E.g., a person with signs of hyposalivation may not complain of xerostomia. Conversely a person who reports experiencing xerostomia may not show signs of reduced salivary secretions (subjective xerostomia).[8] In the latter scenario, there are often other oral symptoms suggestive of oral dysesthesia ("burning mouth syndrome").[3] Some symptoms outside the mouth may occur together with xerostomia. These include:
- Xerophthalmia (dry eyes).[1]
- Inability to cry.[1]
- Blurred vision.[1]
- Photophobia (light intolerance).[1]
- Dryness of other mucosae, e.g., nasal, laryngeal, and/or genital.[1]
- Burning sensation.[1]
- Itching or grittiness.[1]
- Dysphonia (voice changes).[1]
There may also be other systemic signs and symptoms if there is an underlying cause such as Sjögren's syndrome,[1] for example, joint pain due to associated rheumatoid arthritis.
Differential diagnosis
The differential of hyposalivation significantly overlaps with that of xerostomia. A reduction in saliva production to about 50% of the normal unstimulated level will usually result in the sensation of dry mouth.[8] Altered saliva composition may also be responsible for xerostomia.[8]
Physiologic
Salivary flow rate is decreased during sleep, which may lead to a transient sensation of dry mouth upon waking. This disappears with eating or drinking or with oral hygiene. When associated with halitosis, this is sometimes termed "morning breath". Dry mouth is also a common sensation during periods of anxiety, probably owing to enhanced sympathetic drive.[11] Dehydration is known to cause hyposalivation,[1] the result of the body trying to conserve fluid. Physiologic age-related changes in salivary gland tissues may lead to a modest reduction in salivary output and partially explain the increased prevalence of xerostomia in older people.[1] However, polypharmacy is thought to be the major cause in this group, with no significant decreases in salivary flow rate being likely to occur through aging alone.[9][12]
Drug induced
| Medications associated with xerostomia (with or without objective hyposalivation and/or altered saliva consistency).[1] |
|---|
|
Aside from physiologic causes of xerostomia, iatrogenic effects of medications are the most common cause.[1] A medication which is known to cause xerostomia may be termed xerogenic.[3] Over 500 medications produce xerostomia as a side effect (see table).[9] Sixty-three percent of the top 200 most commonly prescribed drugs in the United States are xerogenic.[9] The likelihood of xerostomia increases in relation to the total number of medications taken, whether the individual medications are xerogenic or not.[9] The sensation of dryness usually starts shortly after starting the offending medication or after increasing the dose.[1] Anticholinergic, sympathomimetic, or diuretic drugs are usually responsible.[1]
Sjögren's syndrome
Xerostomia may be caused by autoimmune damage to the salivary glands. Sjögren's syndrome is one such disease, and it causes other symptoms, including xerophthalmia (dry eyes), dry vagina, fatigue, myalgia (muscle pain), and arthralgia (joint pain). Females are more likely to suffer from autoimmune disease, and 90% of people with Sjögren's syndrome are women. Primary Sjögren's syndrome is the combination of dry eyes and xerostomia. Secondary Sjögren's syndrome is identical to primary form but with the addition of a combination of other connective tissue disorders such as systemic lupus erythematosus or rheumatoid arthritis.[8]
Sicca syndrome
"Sicca" simply means dryness. Sicca syndrome is not a specific condition, and there are varying definitions, but the term can describe oral and eye dryness that is not caused by autoimmune diseases (e.g. Sjogren Syndrome).
Other causes
Oral dryness may also be caused by mouth breathing,[3] usually caused by partial obstruction of the upper respiratory tract. Examples include hemorrhage, vomiting, diarrhea, and fever.[1][9] Irradiation of the salivary glands often causes profound hyposalivation.[1] Alcohol may be involved in the etiology as a cause of salivary gland disease, liver disease, or dehydration.[3] Smoking is another possible cause.[9] Other recreational drugs such as methamphetamine,[13] cannabis,[14] hallucinogens,[15] or heroin,[16] may be implicated. Rarer causes include diabetes (dehydration),[1] hyperparathyroidism,[1] cholinergic dysfunction (either congenital or autoimmune),[1] salivary gland aplasia or atresia,[3] sarcoidosis,[3] human immunodeficiency virus infection (due to antiretroviral therapy, but also possibly diffuse infiltrative lymphocytosis syndrome),[1][3][8] graft-versus-host disease,[3] renal failure,[3] hepatitis C virus infection,[8] and Lambert-Eaton syndrome.[17]
Diagnostic approach
A diagnosis of hyposalivation is based predominantly on the clinical signs and symptoms.[1] There is little correlation between symptoms and objective tests of salivary flow,[18] such as sialometry. This test is simple and noninvasive, and involves measurement of all the saliva a patient can produce during a certain time, achieved by dribbling into a container. Sialometery can yield measures of stimulated salivary flow or unstimulated salivary flow. Stimulated salivary flow rate is calculated using a stimulant such as 10% citric acid dropped onto the tongue, and collection of all the saliva that flows from one of the parotid papillae over five or ten minutes. Unstimulated whole saliva flow rate more closely correlates with symptoms of xerostomia than stimulated salivary flow rate.[1] Sialography involves introduction of radio-opaque dye such as iodine into the duct of a salivary gland.[1] It may show blockage of a duct due to a calculus. Salivary scintiscanning using technetium is rarely used. Other medical imaging that may be involved in the investigation include chest x-ray (to exclude sarcoidosis), ultrasonography and magnetic resonance imaging (to exclude Sjögren's syndrome or neoplasia).[1] A minor salivary gland biopsy, usually taken from the lip,[19] may be carried out if there is a suspicion of organic disease of the salivary glands.[1] Blood tests and urinalysis may be involved to exclude a number of possible causes.[1] To investigate xerophthalmia, the Schirmer test of lacrimal flow may be indicated.[1] Slit-lamp examination may also be carried out.[1]
Treatment
The successful treatment of xerostomia is difficult to achieve and often unsatisfactory.[9] This involves finding any correctable cause and removing it if possible, but in many cases it is not possible to correct the xerostomia itself, and treatment is symptomatic, and also focuses on preventing tooth decay through improving oral hygiene. Where the symptom is caused by hyposalivation secondary to underlying chronic disease, xerostomia can be considered permanent or even progressive.[8] The management of salivary gland dysfunction may involve the use of saliva substitutes and/or saliva stimulants:[6]
- Saliva substitutes – these include water, artificial salivas (mucin-based, carboxymethylcellulose-based), and other substances (milk, vegetable oil).
- Saliva stimulants – organic acids (ascorbic acid, malic acid), chewing gum, parasympathomimetic drugs (choline esters, e.g. pilocarpine hydrochloride, cholinesterase inhibitors), and other substances (sugar-free mints, nicotinamide).
Saliva substitutes can improve xerostomia, but tend not to improve the other problems associated with salivary gland dysfunction.[6] Saliva stimulants may improve xerostomia symptoms and other problems associated with salivary gland dysfunction, and patients find them more effective than saliva substitutes.[6] Salivary stimulants are probably only useful in people with some remaining detectable salivary function.[3] A drug or substance that increases the rate of salivary flow is termed a sialogogue. A systematic review of the treatment of dry mouth found no strong evidence to suggest that a specific topical therapy is effective.[8] The review reported limited evidence that oxygenated glycerol triester spray was more effective than electrolyte sprays.[8] Sugar free chewing gum increases saliva production but there is no strong evidence that it improves symptoms.[8] There is a suggestion that intraoral devices and integrated mouthcare systems may be effective in reducing symptoms, but there was a lack of strong evidence.[8] A systematic review of the management of radiotherapy induced xerostomia with parasympathomimetic drugs found that there was limited evidence to support the use of pilocarpine in the treatment of radiation-induced salivary gland dysfunction.[6] It was suggested that, barring any contraindications, a trial of the drug be offered in the above group (at a dose of five mg three times per day to minimize side effects).[6] Improvements can take up to twelve weeks.[6] However, pilocarpine is not always successful in improving xerostomia symptoms.[6] The review also concluded that there was little evidence to support the use of other parasympathomimetics in this group.[6]
Epidemiology
Xerostomia is a very common symptom. A conservative estimate of prevalence is about 20% in the general population, with increased prevalences in females (up to 30%) and the elderly (up to 50%).[8]
History
Xerostomia has been used as a test to detect lies, which relied on emotional inhibition of salivary secretions to indicate possible incrimination.[20]
See also
- Xerosis (dry skin)
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 Scully, Crispian (2008). Oral and maxillofacial medicine : the basis of diagnosis and treatment (2nd ed.). Edinburgh: Churchill Livingstone. pp. 17, 31, 41, 79–85. ISBN 9780443068188.
- ↑ Wijers OB, Levendag PC, Braaksma MM, Boonzaaijer M, Visch LL, Schmitz PI (2002), "Patients with head and neck cancer cured by radiation therapy: a survey of the dry mouth syndrome in long-term survivors", Head Neck, 24 (8): 737–747, doi:10.1002/hed.10129, PMID 12203798.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 Tyldesley, Anne Field, Lesley Longman in collaboration with William R. (2003). Tyldesley's Oral medicine (5th ed.). Oxford: Oxford University Press. pp. 19, 90–93. ISBN 0192631470.
- ↑ "Etymology of "xeros" at Online Etymology Dictionary". Douglas Harper. Retrieved 9 February 2013.
- ↑ "Etymology of "stoma" at Online Etymology Dictionary". Douglas Harper. Retrieved 9 February 2013.
- 1 2 3 4 5 6 7 8 9 10 11 Davies, AN; Shorthose, K (Jul 18, 2007). Davies, Andrew N, ed. "Parasympathomimetic drugs for the treatment of salivary gland dysfunction due to radiotherapy". Cochrane database of systematic reviews (Online) (3): CD003782. doi:10.1002/14651858.CD003782.pub2. PMID 17636736.
- 1 2 3 Coulthard, Paul; et al. (2008). Oral and Maxillofacial Surgery, Radiology, Pathology and Oral Medicine (2nd ed.). Edinburgh: Churchill Livingstone/Elsevier. pp. 210, 212–213. ISBN 9780443068966.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 Furness, S; Worthington, HV; Bryan, G; Birchenough, S; McMillan, R (Dec 7, 2011). Furness, Susan, ed. "Interventions for the management of dry mouth: topical therapies". Cochrane database of systematic reviews (Online) (12): CD008934. doi:10.1002/14651858.CD008934.pub2. PMID 22161442.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Bouquot, Brad W. Neville , Douglas D. Damm, Carl M. Allen, Jerry E. (2002). Oral & maxillofacial pathology (2. ed.). Philadelphia: W.B. Saunders. pp. 398–399. ISBN 0721690033.
- ↑ Hara, AT; Zero, DT (2014). "The potential of saliva in protecting against dental erosion.". Monographs in oral science. 25: 197–205. doi:10.1159/000360372. PMID 24993267.
- ↑ Boyce, HW; Bakheet, MR (February 2005). "Sialorrhea: a review of a vexing, often unrecognized sign of oropharyngeal and esophageal disease". Journal of Clinical Gastroenterology. 39 (2): 89–97. PMID 15681902.
- ↑ Turner MD, Ship JA (September 2007). "Dry mouth and its effects on the oral health of elderly people". Journal of the American Dental Association (1939). 138 (1): 15S–20S. doi:10.14219/jada.archive.2007.0358. PMID 17761841.
- ↑ Saini, T; Edwards, PC; Kimmes, NS; Carroll, LR; Shaner, JW; Dowd, FJ (2005). "Etiology of xerostomia and dental caries among methamphetamine abusers". Oral health & preventive dentistry. 3 (3): 189–95. PMID 16355653.
- ↑ Versteeg, PA; Slot, DE; van der Velden, U; van der Weijden, GA (Nov 2008). "Effect of cannabis usage on the oral environment: a review". International journal of dental hygiene. 6 (4): 315–20. doi:10.1111/j.1601-5037.2008.00301.x. PMID 19138182.
- ↑ Fazzi, M; Vescovi, P; Savi, A; Manfredi, M; Peracchia, M (October 1999). "[The effects of drugs on the oral cavity]". Minerva stomatologica. 48 (10): 485–92. PMID 10726452.
- ↑ "DrugFacts: Heroin on National Institute of Drug Abuse". National Institutes of Health. Retrieved 9 February 2013.
- ↑ Newsom-Davis, J (February 2004). "Lambert-Eaton myasthenic syndrome". Revue neurologique. 160 (2): 177–80. doi:10.1016/S0035-3787(04)70888-7. PMID 15034474.
- ↑ Visvanathan, V; Nix, P (February 2010). "Managing the patient presenting with xerostomia: a review". International journal of clinical practice. 64 (3): 404–7. doi:10.1111/j.1742-1241.2009.02132.x. PMID 19817913.
- ↑ Fox, PC; van der Ven, PF; Sonies, BC; Weiffenbach, JM; Baum, BJ (April 1985). "Xerostomia: evaluation of a symptom with increasing significance". Journal of the American Dental Association (1939). 110 (4): 519–25. PMID 3858368.
- ↑ Iorgulescu, G (Jul–Sep 2009). "Saliva between normal and pathological. Important factors in determining systemic and oral health". Journal of medicine and life. 2 (3): 303–7. PMID 20112475.